Audit
- clinical audit is the systematic and critical analysis of the quality of clinical care
- includes the procedures used for diagnosis and treatment, the associated use of resources and the effect of care on the outcome and quality of life for the patient.
- the definition endorsed by NICE is that '...Clinical audit is a quality improvement process that seeks to improve the patient care and outcomes through systematic review of care against explicit criteria and the implementation of change. Aspects of the structures, processes and outcomes of care are selected and systematically evaluated against explicit criteria. Where indicated, changes are implemented at an individual team, or service level and further monitoring is used to confirm improvement in healthcare delivery....'.
Clinical audit is recognized as having three elements:
- 1. Measurement - measuring a specific element of clinical practice
- 2. Comparison - comparing results with the recognized standard
- 3. Evaluation - reflecting on outcome of audit and where indicated, changing practice accordingly
Purpose of audit
- the objective of audit is to measure and improve performance but its results are not necessarily generalisable (applicable) to other practices.
- audit usually aims to influence activity at a local level
- audit assumes that standards, guidelines or evidence supporting best practice exist and involves the comparison of current practice to these; hence it seeks to determine if we are doing what we should be doing
What audit is not (3)
- Not about:
- Performance Appraisal of Staff
- Disciplinary Actions
- Needs Assessment
- Research (which is usually about establishing new knowledge)
- Computers and Statistics
- Competition between doctors
- "Never judge good and bad professionals based on audit" - it is about improving care
Clinical audit can:
- Provide evidence of current practice against national/international guidelines or quality improvement standards
- Provide information about the structures, the processes or outcomes of a service
- Assess how closely local practice resembles recommended practice
- Establish if you are actually doing what you think you are doing
- Provide evidence/assurance about the quality of care Identify major risk, resource and service development implications
- Reinforce implementation of evidence-based practice Influence improvements to individual patient care
If you are considering whether the task to be undertaken is an audit or a research project - the the decision tree below is helpful in deciding between these two tasks:
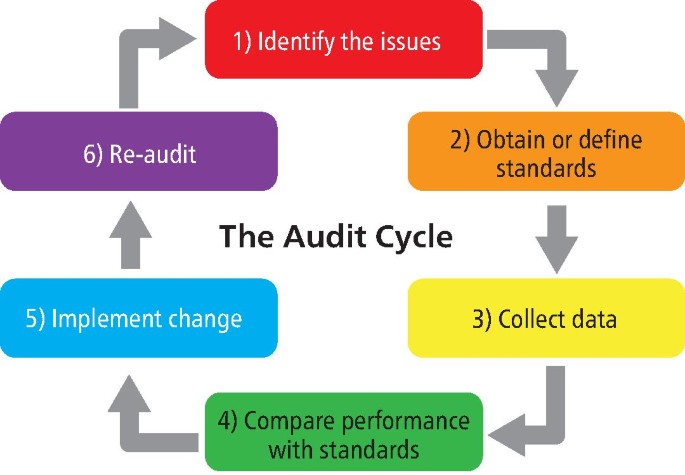
The audit cycle
- Stage 1 - preparation
- Choose a topic:
- should be one which is a high priority for your organisation
- may involve areas in which there is a high volume of work, high risks or high costs of care, or an area identified as a priority by patients.
- identify available resources
- there may be an audit lead or office in your organisation
- may be existing guidelines defining desired standards for the topic you have chosen
- Stage 2 - select criteria
- Define the criteria
- in the form of a statement
- all patients initiated on ACE inhibitors should have their renal biochemistry checked within two weeks of initation
- Define the standard
- usually a target (percentage)
- may be a minimum standard or an optimal one, depending on the clinical scenario
- Stage 3 - measuring level of performance
- Collection of data
- from computerised records, manual collection, or both
- retrospective or prospective
- Analyse the data collected:
- Compare actual performance with the set standard
- Discuss how well the standards were met
- If the standards were not met, note the reasons for this (if known)
- Stage 4 - making improvements
- Present the results and discuss them with the relevant teams in your organisation.
- The results should be used to develop an action plan, specifying what needs to be done, how it will be done, who is going to do it and by when
- Stage 5 - maintaining improvements
- follows up the previous stages of the audit, to determine whether the actions taken have been effective, or whether further improvements are needed
- involves repeating the audit (ie targets, results, discussion); hence the terms 'audit cycle'
Definitions
- Criterion:
- definable measurable item of healthcare that describes quality and which can be used to assess it, eg the number of people with diabetes who have had their lipids checked within the last one year
- often best expressed as a statement, eg 'All patients with coronary heart disease should have had their lipids checked annually'
- should be evidence-based wherever possible
- Standard:
- the level of care to be achieved for any particular criterion
- in some instances then the standard chosen might be 100% (for example the number of patients initiated on an ACE inhibitor who had their renal biochemistry rechecked within two weeks of initiation of an ACE inhibitor) - for other criterion then lower standards may be appropriate.