FRAILTY.
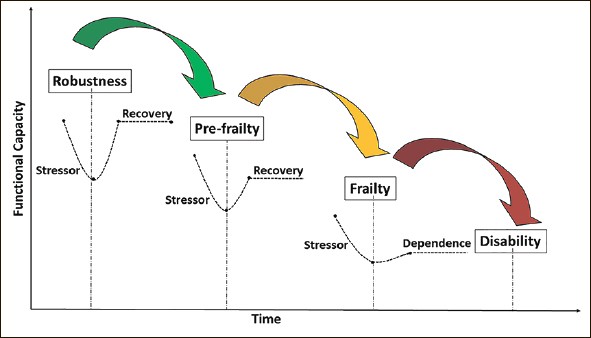
- Vulnerability to adverse outcomes
- Poor response to stressors
- Unstable homeostasis.
Hard to define but easy to recognise!
It is dynamic- may need multiple components assessed over time.
It is not the same as disability·
Fits well into bio-psycho-social model of general practice.
Allows identifications by simple scales
Allows resources to be directed efficiently
Be reversed or slowed along its continuum.
- 7%at 60
- 20-40% at 80 years.
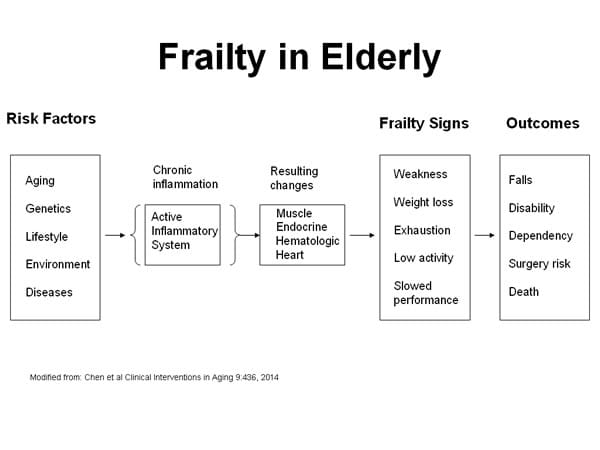
- Disability increased.
- Falls increased.
- Admissions to acute or continuing care increased.
- Reluced quality of life.
- Increased risk of medicine se
- Increased death rates – better indicator of death than age.
- Implications to State.
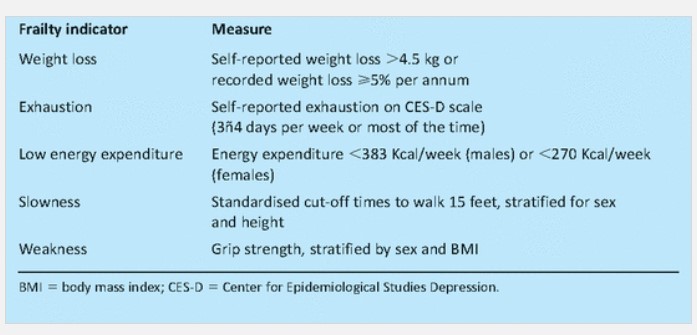
Measurability.
Core elements - any 3.
- Weakness (grip strength).
- Tiredness.
- Weight loss(10 pounds in 6 months)
- Poor endurance / energy’·
- Reduced physical activity levels.
- Slow gait speed.
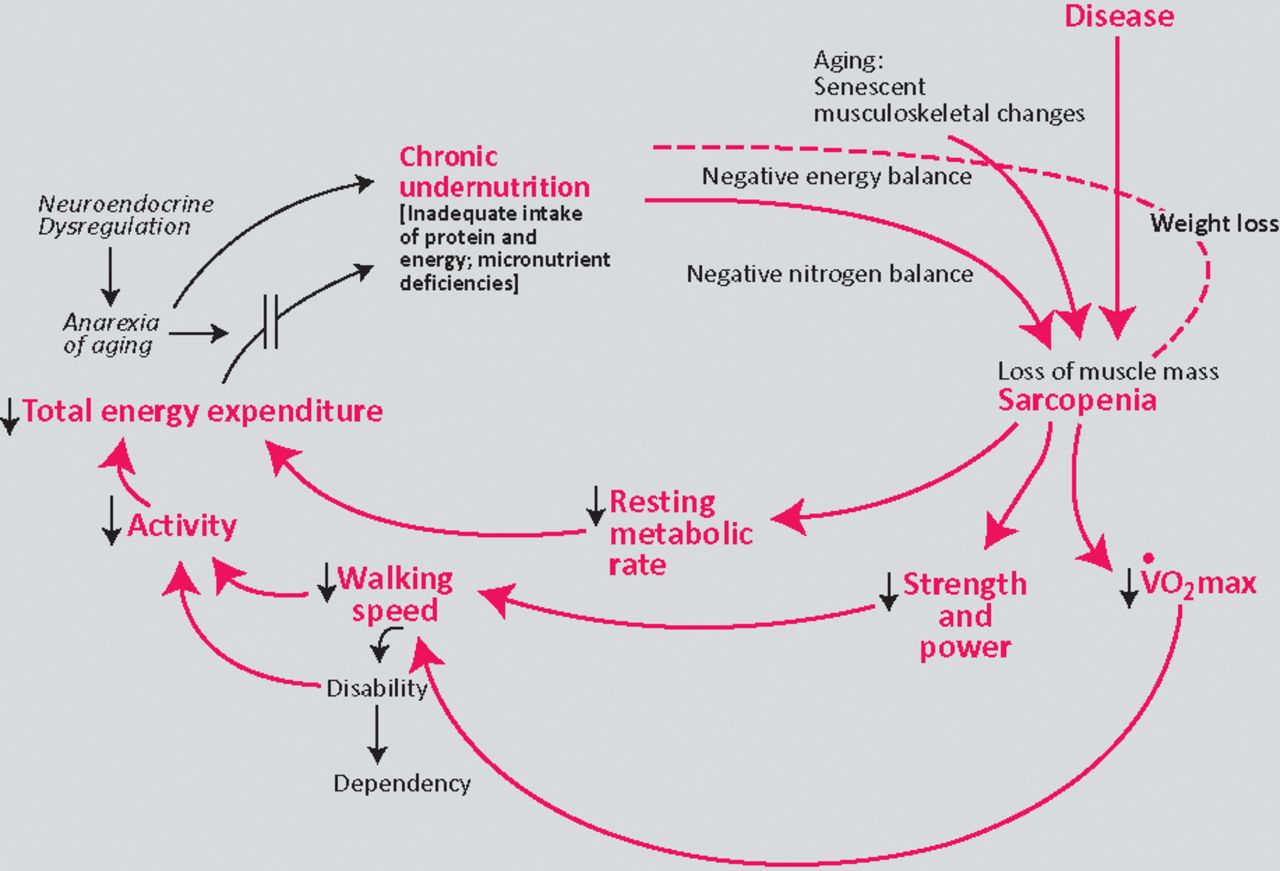
Causes.- .
- Aging .. but not universal.
- Anorexia/ underweight.
- Immobility°
- Atherosclerosis.
- Depression.
- Cognitive impairment
- Loss of balance.
- Sarcopenia – loss of lean body mass.
Challenges
- Health service is reactive and fragmented.
- Doctors trained in medical model, organ / disease specific.
- Aging population, decreasing resources.
Treatment is holistic.
- Managing all underlying medical illnesses.
- Avoid medication toxicity.
- Prevent muscle mass loss.
- Depression / dementia recognition.
F Food
R Resistance exercise, 3 / week
A Atherosclerosis prevention
I Isolation avoidance.
L Limit pain.
T tai chi!
Y yearly review, inc bloods ( testosterone in men).